Call 1300 849 118
Weight Loss Surgery - Single Anastomosis Bypass
What is a Mini Gastric Bypass?
Do I Qualify for a Gastric Bypass?
Single Anastomosis Gastric Bypass Procedure
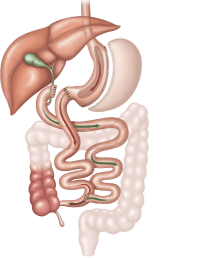
The SAGB procedure is performed with a laparoscopic (keyhole) technique under general anaesthesia.
- The upper part of the stomach is divided into a tube, similar to the top three-quarters of a sleeve and then joined to a loop of intestine.
- Five small incisions (between 5 and 12mm in length) are made for the insertion of keyhole surgery instruments.
- Using these instruments, the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach and is completely separate to the rest of the stomach.
- This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150-200cm of the bowel. The rest of the stomach and upper part of the small intestine remains in the body but is no longer used for food digestion.
How Does Single Anastomosis Gastric Bypass Work
- Restricting the amount of food that can be eaten at any one time, thereby reducing meals to healthy portion size, and
- Decreasing the number of calories your body absorbs during digestion as food bypass about 200cm of your upper small intestine
Expected Weight Loss
Advantages of a Gastric Bypass
- It is particularly effective for patients with a larger BMI as the procedure has more predictable weight loss outcomes.
- Most patients have an almost immediate reduction in their need for diabetic medication and some are able to completely stop diabetic medication altogether.
- It does not require any on-going adjustments which are required with other procedures, such as the gastric band. Regular follow up is however necessary to ensure weight loss is appropriate and intake is nutritionally adequate.
- It is effective for those people who tend towards high sugar or high-fat foods. Dumping syndrome is directly linked to a high-sugar, or high-fat intake. Symptoms of dumping are unpleasant and therefore discourage the intake of high-calorie sweet foods.
Disadvantages of a Gastric Bypass
- Complications, although rare, are generally more serious than with other weight loss procedures, such as the gastric band.
- There is a higher risk of nutritional deficiency due to the reduced absorption of vitamins and nutrients. Life-long vitamin and mineral supplementation is essential to prevent deficiency following surgery. Long term follow-ups with the surgeon and dietitian to monitor nutritional status is also very important.
Risks of a Gastric Bypass
Possible Acute Complications
- Bleeding - this occurs in less than 1 in 100 patients after the procedure. This may require blood transfusion or rarely reoperation.
- Infection – if an infection develops it may require treatment with antibiotics and can occasionally require reoperation.
- Leak - a leak of fluid can occur through the new join between the stomach and intestines if it does not heal well. This can happen in the first few days after surgery and may require reoperation. If these leaks persist they can leak to the skin or wound (known as a fistula) or cause a persistent fluid infection in the area (abscess). If this happens, length of hospital stay may be extended to weeks or even months after surgery, and it may be a life-threatening problem. This occurs in less than 1% of cases.
- Ulcers - Just like ulcers can occur in a normal stomach, they can also occur in the new stomach pouch after a gastric bypass. For this reason, patients need to take anti-ulcer medication for 6 months after surgery. Sometimes ulcers can still develop and require additional therapy to manage.
- Damage to Organs – any keyhole procedure can be complicated by unintentional injury to the organs near the area of operation. This may require a repeat operation to repair the damaged organs.
- Blood Clots – Deep Venous Thromboses (clots in the veins) and pulmonary embolus (clots in the lungs)
- Pneumonia/ Chest Infection
- We take measures directly aimed at reducing these risks, but if complications occur, additional treatment may be necessary.
Possible Long-Term Complications
- Wound Hernia – any wound of the abdominal wall has a chance, anytime in future, of developing a hernia (some of the bowel or fat from inside the abdomen can get stuck underneath the skin). If this happens it needs to be assessed, and if it is red, hot and painful it should be seen to quickly as it may be an emergency.
- Anastomotic Stricture – It is important to keep the new connection between the stomach and the intestines small so as to achieve the right amount of weight loss. Sometimes this means the connection is too tight (less than 1 in 10 patients). If this occurs it may require stretching under endoscopy (camera into the stomach).
- Internal Hernia – occasionally the loops of bowel in the abdomen can become entangled and get stuck. If this occurs, a re-operation is required to fix the problem. If there are any unexpected abdominal complaints it is important to be assessed quickly by the surgeon.
- Adhesions – any procedure in the abdomen can cause adhesions (scar tissue). This can occur any time after the operation and can sometimes cause problems with the bowel getting stuck or twisted. This may require hospitalization and may even require re-operation.
- Gastro-Oesophageal Reflux – If reflux occurs post-operatively some patients can require acid-suppressing medication. This operation should be avoided for those people with severe symptoms of reflux prior to surgery.
- Failure of weight loss/weight regain – this usually occurs when dietary advice is not followed. If you eat too much food at once this can stretch the small stomach pouch making it easier to take larger volumes at meal times in the future.
- Other - As this surgery affects the function of the gut, some patients are unable to tolerate adequate intakes of food which can result in the requirement of long-term nutritional support via intravenous methods, called TPN (total parenteral nutrition).
Dumping Syndrome
Pre-Operative Diet
Post-Operative Care
Surgeon
Dietitian
CONSULTING LOCATIONS
- St George Private Hospital 1 South St, Kogarah, 2217, New South Wales, Australia
- Figtree Private Hospital 1 Suttor Pl, Figtree, 2525, NSW, Australia
- Sydney South West Private Hospital 24 Bigge St, Liverpool, NSW, Australia
- Coffs Harbour 53 Moonee Street, Coffs Harbour New South Wales 2450, Australia
- Windsor 267 George Street, Windsor New South Wales 2756, Australia
HOSPITAL LOCATIONS
About Us
Our focus is on helping our patients lose weight and stay a healthy weight thereafter. Read more about us...
Clinics at
Dr Jason Maani is not a financial service provider. The information provided regarding payment options, including private health funds, superannuation access, and other financial assistance services, is for information purposes only. These services are independent of Dr Jason Maani, and patients are responsible for directly contacting the relevant providers to understand the terms, eligibility, and process for utilising these options for their procedure costs. Dr Jason Maani does not provide financial or insurance advice and recommends patients seek independent financial or professional advice regarding payment methods.